Hospital at Home in Germany: opportunities, challenges & prospects
Hospital at Home in Germany: opportunities, challenges & prospects
In Germany, discharge from hospital often marks the end of care. The patient is discharged into a vacuum characterised by unclear responsibilities, a lack of control and high relapse rates. For hospitals, this means unnecessary readmissions, rising costs and dissatisfied patients.
But there has long been a better solution - both medically and economically:
Telemedizinische Technologien und Hospital-at-Home-Programme füllen das Vakuum zwischen stationärer und ambulanter Versorgung.

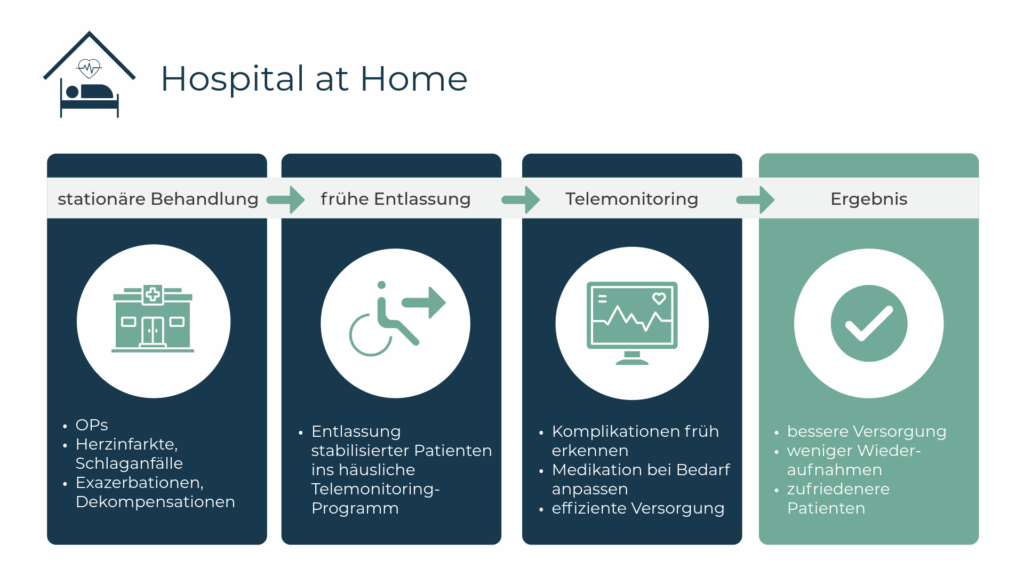
Hospital-at-Home: Clinical control without a hospital bed
The challenges in everyday hospital life are well known: rising patient numbers, a shortage of skilled staff, limited bed capacity. At the same time, hospitals need to ensure a high quality of care - not only during the inpatient stay, but also afterwards.
Genau hier setzt Hospital-at-Home-Konzept an. Es verbindet drei Säulen zu einem care model equivalent to inpatient care in the home:
1. telemonitoring
2. televisits
3. outpatient care
- Digital surveillance (Telemonitoring): Depending on the illness, vital parameters such as blood pressure, pulse or lung function are continuously recorded by the patient and transmitted to the clinic. Automatic alarms are triggered immediately if values become critical.
- Televisits: Regular televisits enable a direct exchange between medical staff and patients - without travelling, but with clinical care.
- Outpatient support on site: Mobile care services can make home visits, administer medication or provide nursing care if required.
The result: Hospital-at-Home enables close-knit, intersectoral and efficient digital aftercare - without a hospital bed, but with clinical standards.
3 reasons why clinics should focus on digital care models now
- The future of patient care is hybrid
Telemedical hospital-at-home programmes enable modern, patient-centred care that brings hospital standards into the living room. Those who invest today are positioning themselves as pioneers in a healthcare system that is increasingly focussing on outpatient, digital and flexible care models.
- Resource bottlenecks in clinics require new care pathways
In the face of cost pressure, a shortage of specialist staff and overcrowded hospitals, telemonitoring programmes offer an effective way of conserving inpatient capacity without compromising on quality. Telemonitoring ensures safety and control - even outside the hospital walls.
- Sector boundaries can be overcome digitally
Digital care models such as hospital-at-home promote close collaboration between hospitals, GP practices and outpatient services. Structured task planning and the digital exchange of relevant health data create a seamless flow of information - for more efficient care without frictional losses at the interfaces.
Telemedicine in hospitals: 2 examples from Germany
Example 1:
The Telemedicine centre of the Robert Bosch Hospital cares for patients with chronic heart failure and COPD. The combination of vital data monitoring and personal telephone support enables close follow-up care - with positive effects on quality of life and security of care.
Example 2:
The Institute for Applied Telemedicine (IFAT) of the Heart and Diabetes Centre NRW (University Hospital of the Ruhr University Bochum) cares for around 11,000 patients with telemedical services.
With a newly installed telemedical programme for the care of heart patients the Institute is setting new standards in telemonitoring for heart failure.
3 ways to finance hospital-at-home in Germany
The implementation of telemedicine hospital-at-home programmes can be realised in Germany via various funding channels - depending on the strategic focus and healthcare context:
Regular outpatient HI care via an MVZ
In Germany, telemedical care has so far become part of standard outpatient care for one group of patients: the Telemonitoring for chronic heart failure. This approach is ideal for clinics that work closely with an MVZ and want to transfer inpatients to long-term outpatient care via telemonitoring after discharge.
Selective contracts with health insurance companies
Clinics and health insurance companies can agree customised care models via individual selective contracts. These contracts offer flexibility in the design of services, remuneration and quality criteria - ideal for innovative hospital-at-home programmes that go beyond standard care. They also enable close cooperation between service providers and payers.
Funding via the KHTF (cross-indication)
The Hospital Transformation Fund (KHTF) offers a strategically particularly relevant funding opportunity for the structured development of telemedical networks. The central element here is the subsidisation criteria in accordance with Section 3 (3) KHTFV for the establishment of telemedical network structures.
This subsidy provides targeted support:
- The creation of cross-sector telemedical infrastructures
- The establishment of digital supply chains between hospitals, community-based doctors and outpatient services
- Investments in interoperable telemonitoring systems and digital communication platforms
The decisive advantage: The funding is designed to be cross-indication - hospital-at-home structures can therefore be created in various specialist areas of clinical aftercare. This creates sustainable, future-proof care structures that go beyond individual clinical pictures.
Hospitals that take a strategic approach to setting up telemedicine networks now will not only secure funding, but also position themselves as key players in networked, digital healthcare.
Source:
1 Federal Ministry of Health: Hospital Care Improvement Act (KHVVG)
Into the future of clinical aftercare
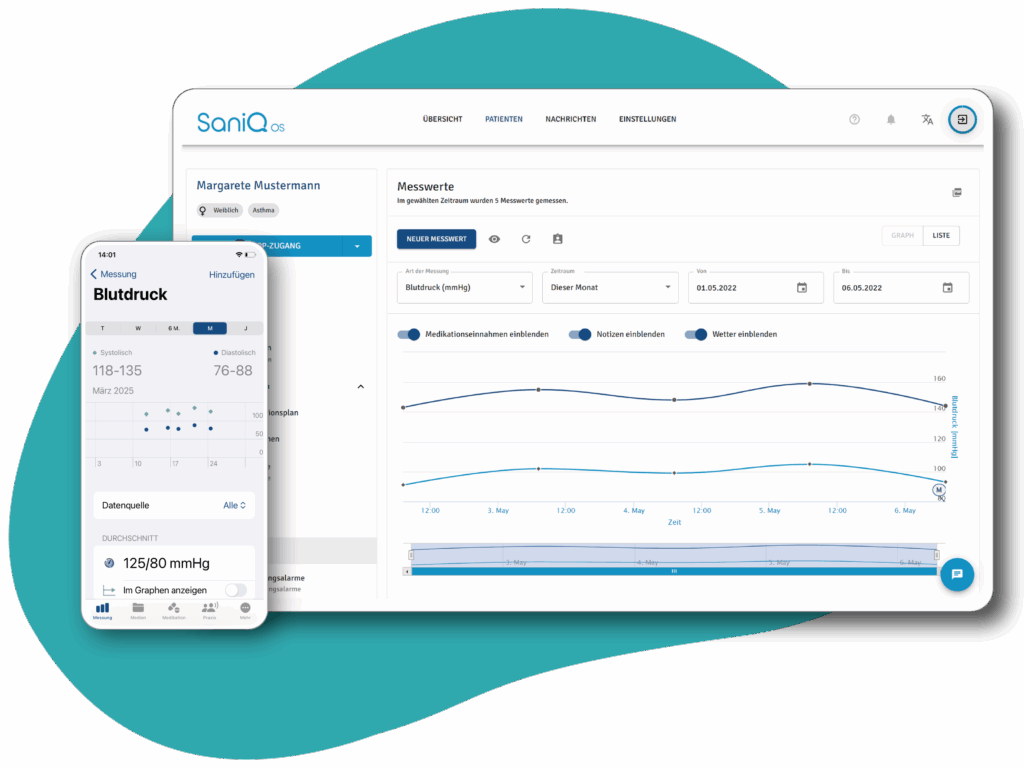
The SaniQ OS telemedicine platform enables clinics to provide structured, digital aftercare - for earlier discharges, fewer readmissions and more satisfied patients.
These articles might be of interest to you:

Future check: Telemonitoring in Germany
As a key digital medical technology, telemonitoring is central to overcoming urgent challenges in the German healthcare system. So where does Germany stand when it comes to integrating this pioneering technology into healthcare?

How digital medicine is closing the care gap for rare diseases
Innovative telemedicine applications can significantly improve the care of people with rare diseases. A team of doctors at Berlin's Charité hospital is breaking new ground to provide much-needed support to those affected by a neurological disease.
