Remote Patient Monitoring for COPD
Remote Patient Monitoring for COPD
When will Remote Patient Monitoring for COPD become an integral part of standard care? Initial studies were promising - now a study project funded by the G-BA is set to provide clarity. In this article, we shed light on the current state of research and show what a sensible implementation could look like.
When will Remote Patient Monitoring for COPD become an integral part of standard care? Initial studies were promising - now a study project funded by the G-BA is set to provide clarity. In this article, we shed light on the current state of research and show what a sensible implementation could look like.
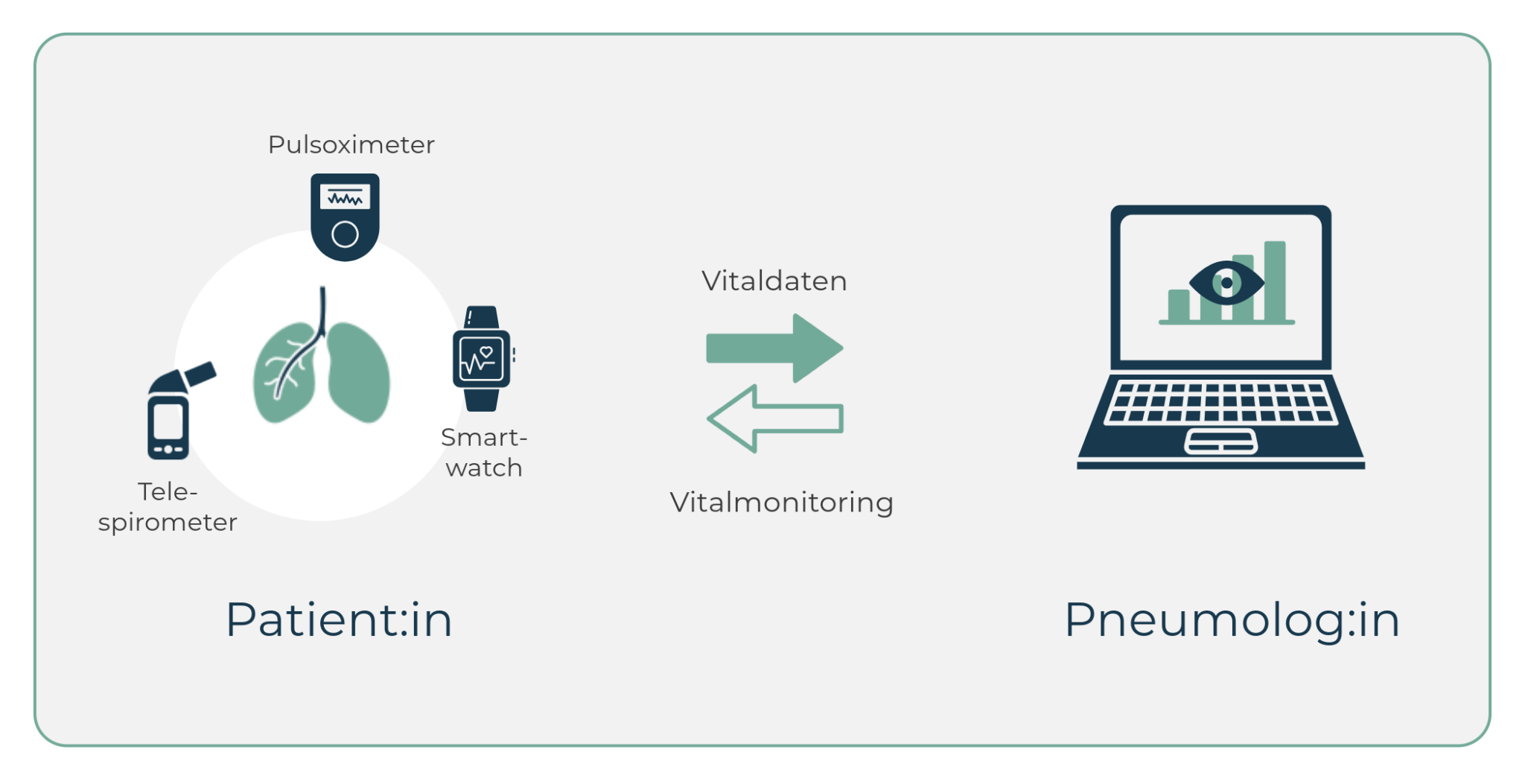
Table of contents
Telemedical care has already proven its worth in cardiology: Since 2022, the Telemonitoring of patients with heart failure a standard benefit of statutory health insurance in Germany.
In view of promising study results on telemonitoring for chronic obstructive pulmonary disease (COPD), one of the most common chronic diseases in Germany, the digital form of care could soon also become standard in pneumology.
Procedure for telemonitoring in COPD
Telemonitoring (also known as remote patient monitoring) for COPD involves the regular remote monitoring of vital signs in order to recognise changes in the patient's state of health at an early stage and be able to intervene. The typical procedure is as follows:
- Data acquisition: Patients measure various parameters (e.g. FEV1, peak flow, heart rate, oxygen saturation) daily or at regular intervals using digitally networked sensor technology.
- Data transmission: The recorded data is automatically transmitted to telemedical software.
- Data analysis: The software's algorithms analyse the incoming data for anomalies or trends that could indicate a deterioration in the condition.
- Alarm system: Medical staff are automatically notified of critical values or trends.
- Intervention: Based on the data, doctors can intervene at an early stage, e.g. by adjusting the medication or calling in the patient.

Which vital signs are suitable for COPD monitoring
Basic parameters:
- Oxygen saturation (SpO2): Enables the assessment of blood oxygenation, particularly important in advanced COPD. Values below 90% are critical and may indicate an exacerbation.
- Peak flow and FEV1: These lung function parameters provide information about airway obstruction. Significant deviations from the personal best value can indicate a deterioration.
- Respiratory rate: An increased respiratory rate (over 20/min at rest) can be an early warning sign of an incipient exacerbation.
Additional parameters:
- Heart rate: Tachycardia may indicate impaired oxygenation or increased physical exertion.
- Blood pressure: Relevant due to frequent cardiovascular comorbidities in COPD patients.
- Body weight: Daily measurement to detect fluid retention or unintentional weight loss.
- Daily step count: Objective indicator of activity level and mobility
Subjective parameters:
- Symptom diary (e.g. dyspnoea, cough, amount and colour of sputum)
- Medication intake, especially frequency of medication on demand
- Activity level and resilience in everyday life
What are the benefits of telemedicine in pneumology?
Several studies show that digital vital signs monitoring can improve the treatment of COPD in various areas:
Medical benefits
- Early detection of exacerbations
- Reduction in hospital stays
- Improved survival rate
Advantages for patients
- Close medical care
- More safety in everyday life
- Improved self-management
Advantages for pneumologists
- Better data basis for treatment decisions
- Efficient form of care relieves pressure on practice operations
- Digital therapy control
Healthcare costs
- Avoided hospital stays and optimised care result in enormous cost savings in the healthcare system

Current study situation
Several studies have already demonstrated significant improvements in care with telemonitoring compared to standard therapy. One of the currently ongoing, most comprehensive studies in this area is the Telementor COPD study, which is being funded by the Federal Joint Committee and is being conducted in Germany.
Telementor-COPD (current study)
The Telementor COPD study is a multicentre, randomised and controlled clinical study funded by the G-BA Innovation Fund and led by the LungenClinic Großhansdorf. It is investigating the benefits of telemedicine and telemonitoring in patients with COPD. For the continuous monitoring of vital signs, the SaniQ telemedicine platform used. The aim is to recognise exacerbations at an early stage and to be able to intervene preventively in good time.
An interim analysis has already indicated promising results. The last patients will complete the study in December 2024 - the results are then expected in spring 2025. They could make a decisive contribution to evaluating the effectiveness of telemonitoring in COPD and to the transition to standard care.
Link to the study: https://innovationsfonds.g-ba.de
Supply study during the coronavirus pandemic (2022)
An app-based care programme at Essen University Hospital for 745 patients with lung diseases such as asthma and COPD showed promising results during the coronavirus pandemic:
The doctors and patients participating in the programme rated the monitoring of central vital signs via smartphone app and Bluetooth spirometer as consistently positive:
- 99% of the participants particularly appreciated the possibility of measuring at home
- 70% of the patients even reported an improved quality of life
- The treating physicians also rated the programme positively and showed a high level of interaction with the digital platform
A promising approach for the future of care for people with respiratory diseases, which could also prove its worth beyond the pandemic.
Link to the study: https://www.springermedizin.de
Study on mortality and healthcare costs (2016)
A study by the Hamburg Centre for Health Economics (HCHE) on the largest European telemonitoring pilot project for COPD patients shows promising results:
- Digital monitoring was able to reduce the mortality rate of participants by around half
- Telemonitoring also led to significant cost savings of an average of 895 euros per patient compared to standard care.
- The effects on patients with severe and very severe COPD were particularly impressive - hospitalisation costs were reduced by more than 1,000 euros.
- The study with over 650 telemonitoring participants also showed that the digitally monitored patients had to visit fewer emergency departments overall and had shorter hospital stays.
Link to the study: link.springer.com
International perspective: Denmark
Denmark is considered a pioneer in the integration of telemedicine into COPD care. Several regional projects (including the TeleCare Nord programme, which was introduced in 2015) have shown what nationwide telemedicine care can look like:
- Continuous monitoring of vital parameters using networked devices.
- Regular video conferences between patients and healthcare professionals.
- A centralised data management system for the early detection of exacerbations.
In November 2023, Denmark announced the introduction of a national telemedicine solution (the Telma platform) for patients with severe chronic obstructive pulmonary disease (COPD) based on the findings of the TeleCare Nord programme. The programme will be rolled out nationwide in 2024.
Conclusion
The legislator has generally recognised the effectiveness of telemonitoring in COPD:
- A transfer to standard care - collectively agreed by the self-administration, the legislator or in selective contracts (§140a SGB V) by the contractual partners - is a declared goal of the G-BA Innovation Fund.
- In this way, the Telementor COPD study will provide important insights into the effectiveness and feasibility of implementation in Germany.
- Experience in Denmark also emphasises the feasibility and benefits of nationwide implementation.
These articles might be of interest to you:

Hospital at Home in Germany: opportunities, challenges and prospects
Discharge from hospital today often marks the end of care. The patient is discharged into a vacuum characterised by unclear responsibilities, a lack of control and high relapse rates. Yet there has long been a better solution - both medically and economically:
Telemonitoring and hospital-at-home programmes fill the vacuum between hospital and home.

Future check: Telemonitoring in Germany
As a key digital medical technology, telemonitoring is central to overcoming urgent challenges in the German healthcare system. So where does Germany stand when it comes to integrating this pioneering technology into healthcare?
