Telemonitoring in Germany
Telemedicine opens up innovative solutions for key challenges facing the German healthcare system. In particular, telemonitoring of patients with common chronic diseases such as heart failure, COPD and diabetes mellitus harbours great potential. But how far has the integration of this key digital technology into German healthcare actually progressed?
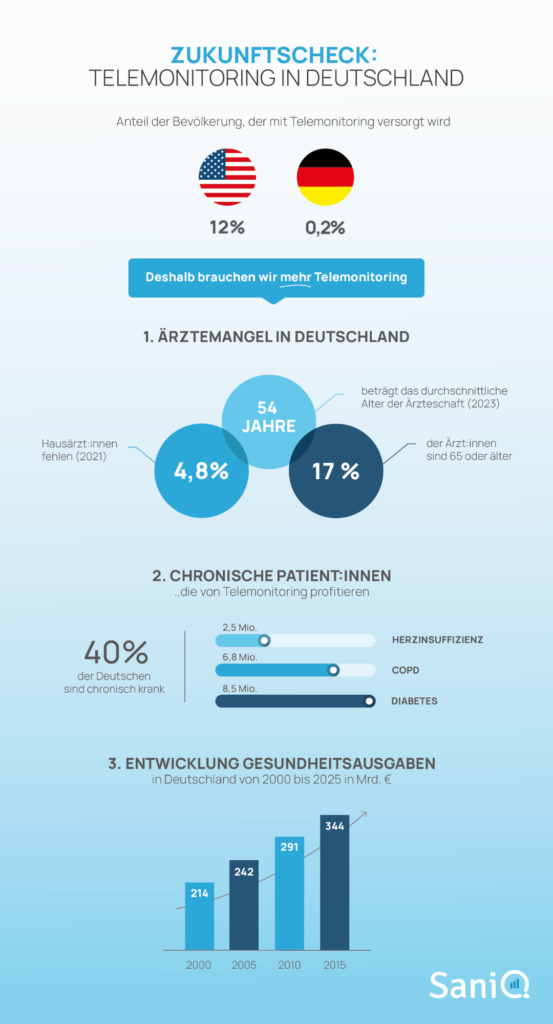
Proportion of the population covered by telemonitoring:

vs.


vs.

In the USA, telemonitoring has become an integral part of medical care for chronically ill people in recent years. The number of patients receiving care increased more than sixfold between 2017 and 2023, from 3 million to 20 million.1
In contrast, Germany has so far only taken hesitant steps towards a digital transformation of the healthcare system. However, digital remote medical monitoring is slowly gaining momentum in this country too.
Definition: What is telemonitoring?
Telemonitoring (also known as remote patient monitoring) is the remote medical monitoring of patients using digital technology. Patients measure relevant vital parameters (e.g. blood pressure, pulse, weight, etc.) on a daily basis in their own home environment using digital sensors, which then transmit them in real time to medical professionals (e.g. a doctor's surgery or a study centre).
The most common areas of application for telemonitoring:
- Chronic diseases such as heart failure, COPD or diabetes
- Postoperative aftercare
- Clinical studies
The health data collected in this way have Positive effects for patients, doctors and the entire healthcare system:
- Support in the early detection of illnesses and critical events
- High density of health data from patients' everyday lives (real world data)
- Increased quality of medical care
- Relief for medical practices in the care of an increasing number of chronic patients
Background
Challenges in the German healthcare system
- Increasing shortage of doctors and specialists (especially in rural areas)
- Demographic development
- Increasing cost pressure
The challenges facing the German healthcare system in the coming years are well known. To make matters worse, the Disease burden of a growing number of chronically ill patientswho require close therapeutic care.
of Germans are chronically ill
Shortage of general practitioners in Germany (as of 2021)
of German doctors are 65 or older
Hybrid supply models as part of the solution?
In light of the challenges mentioned above, there is a growing need for hybrid models that sensibly combine outpatient care structures with digital medical technologies.
In his speech to the Bundestag on the Health Data Utilisation Act and Digital Act on 14 December 2023, Health Minister Karl Lauterbach emphasised the opportunities telemedicine offers in relieving the burden on doctors' surgeries:
The goal: Efficiently manage doctors' capacities while maintaining the quality of outpatient care.
Telemonitoring, i.e. the remote monitoring and care of chronically ill people using digital technology, has enormous potential from an expert's point of view:
"Telemonitoring can be an essential building block for efficient and cross-sectoral care and, if widely utilised, has the potential to support the digital transformation of the healthcare system."
E-Health Monitor 2023 | 24, McKinsey & Company, p. 133

3 Examples: Telemonitoring for chronic diseases
So where does Germany stand with the integration of telemonitoring into healthcare? Using three of the most common chronic diseases in Germany as examples, we show the status of research and the integration of telemedical remote care in the healthcare system.
1. heart failure
Patients in Germany
Deaths in Germany (2022)
Vital signs monitoring (using invasive or external measuring devices)
- Body weight
- ECG
- Blood pressure
Study situation: The medical benefits of telemonitoring in chronic heart failure have been recognised by the German TIM-HF2 study (2011) well documented:
- Reduced complication rate
- Lower risk of cardiovascular-related hospitalisation
- Reduced mortality
A more recent Secondary analysis of the German TIM-HF2 study (2023) shows that the benefit applies to all patients regardless of the severity of the left ventricular pumping function of the heart.
The researchers conclude that standard care with telemonitoring should be extended to all heart failure patients. To date, this has only been provided for a specific group of patients with very limited pumping function (EF<40%).
Integration in the healthcare system:
- The Telemonitoring for chronic heart failure has been part of standard care for high-risk patients in Germany since 2022 following a decision by the Federal Joint Committee. With this decision, Germany is taking on a pioneering role within Europe as the first country to recognise a digital form of care as an independent treatment method.
- However, despite proven evidence and billable EBM codes, only a small proportion of eligible patients have been treated with telemonitoring to date.
- However, cardiological practices that have already started using telemedicine are reporting positive experiences, such as our Case study shows.
2. COPD
Patients in Germany
Deaths in Germany (2022)
Vital signs monitoring:
- One-second air (FEV1)
- Peak flow (PEF)
- Respiratory rate
- Blood oxygen saturation
Study situation:
- In the state subsidised project TELEMENTOR COPD is currently being investigated under the consortium leadership of the LungenClinic Großhansdorf as to whether treatment with the SaniQ telemonitoring platform can reduce the number of relapses (exacerbations).
- An earlier Study during the corona pandemic has already shown positive results in terms of adherence, symptom burden and quality of life of participating patients with bronchial asthma, COPD and SARS-CoV-2.
Integration in the healthcare system:
- Telemonitoring for COPD patients is not yet part of standard care.
- The results of the TELEMENTOR COPD study, which are expected in 2025, could change the situation.
More on the topic
Blog post: Remote Patient Monitoring for COPD
3. diabetes mellitus
Patients in Germany
new diagnoses per year in Germany
Vital signs monitoring:
- Blood sugar levels
- Body weight
- Blood pressure
Study situation:
One published in 2022 Metastudy with 20 analysed studies showed a positive picture. Telemonitoring of patients with type 2 diabetes is associated with the following results:
- Lower blood pressure
- lower BMI
- reduced HbA1c values
With TeLIPro There is also a state-funded project in Germany that combines health coaching for participating patients with type 2 diabetes with telemonitoring of blood glucose levels.
Integration in the healthcare system:
- Telemonitoring for type 2 diabetes is not yet part of standard care.
There are selective contracts with various health insurance companies for the telemonitoring application ESYSTAThe blood glucose values are monitored in connection with injected insulin doses.
Conclusion
In international and European comparison, Germany is still in the early stages of integrating telemonitoring services into treatment practice:
- Heart failure is the only indication in standard care to date
- Ongoing telemonitoring projects are usually regional and limited in time
- There is a lack of quality standards and guidelines for telemonitoring solutions
The inclusion of telemonitoring for heart failure in standard care was an important first step that must now be followed by others.
What is missing?
Incentives for service providers: The inclusion of telemedical care for other illnesses (e.g. asthma, COPD and diabetes) in standard care is overdue. The digital transformation of our healthcare needs more concrete incentives for insured persons and service providers.
Comprehensive supply structure: More information is needed about the opportunities of digitalisation for the healthcare system in order to improve the acceptance of digital innovations among service providers. The goal must be a nationwide service structure that makes improved treatment options accessible to as many patients as possible.
Structures for the digitalisation of care and communication: In addition to telemedical care for individual medical conditions, it would be important to make progress towards the digitalisation of care and communication as a whole - across individual medical conditions. The first steps have already been taken: the Health Data Utilisation Act and the Digital Act of 2023 provide the legal framework that now needs to be filled with life.
Sources:
- McKinsey & Company: E-Health Monitor 2023 | 24 Germany's path to digital healthcare. 2024.
- Kassenärztliche Bundesvereinigung & GKV-Spitzenverband: Quality Assurance Agreement Telemonitoring in Heart Failure. 2022.
- National Association of Statutory Health Insurance Physicians: Doctors in private practice are getting older and older. Online publication 2024.
- Federal Statistical Office.

Remote Patient Monitoring for COPD
When will Remote Patient Monitoring for COPD become an integral part of standard care? Initial studies were promising - now a study project funded by the G-BA is set to provide clarity. In this article, we shed light on the current state of research and show what a sensible implementation could look like.
CME training for practising cardiologists
CME TRAINING Digital perspectives for the cardiology practice: Telemonitoring in chronic heart failure as a telemedicine centre Reserve your place 10 places still available Date:19 November 2025, 4.00 - 7.00 pm
